TLDR: People don't need carbohydrates, ketosis isn't dangerous.
It is pertinent to briefly discuss the enduring misconception that glucose itself represents an “absolutely essential”, “universal fuel” in human physiology, which requires nuanced definition and gradation, but has been perpetuated verbatim and may have been incorporated into the physiology education of currently practicing healthcare professionals [1-7].
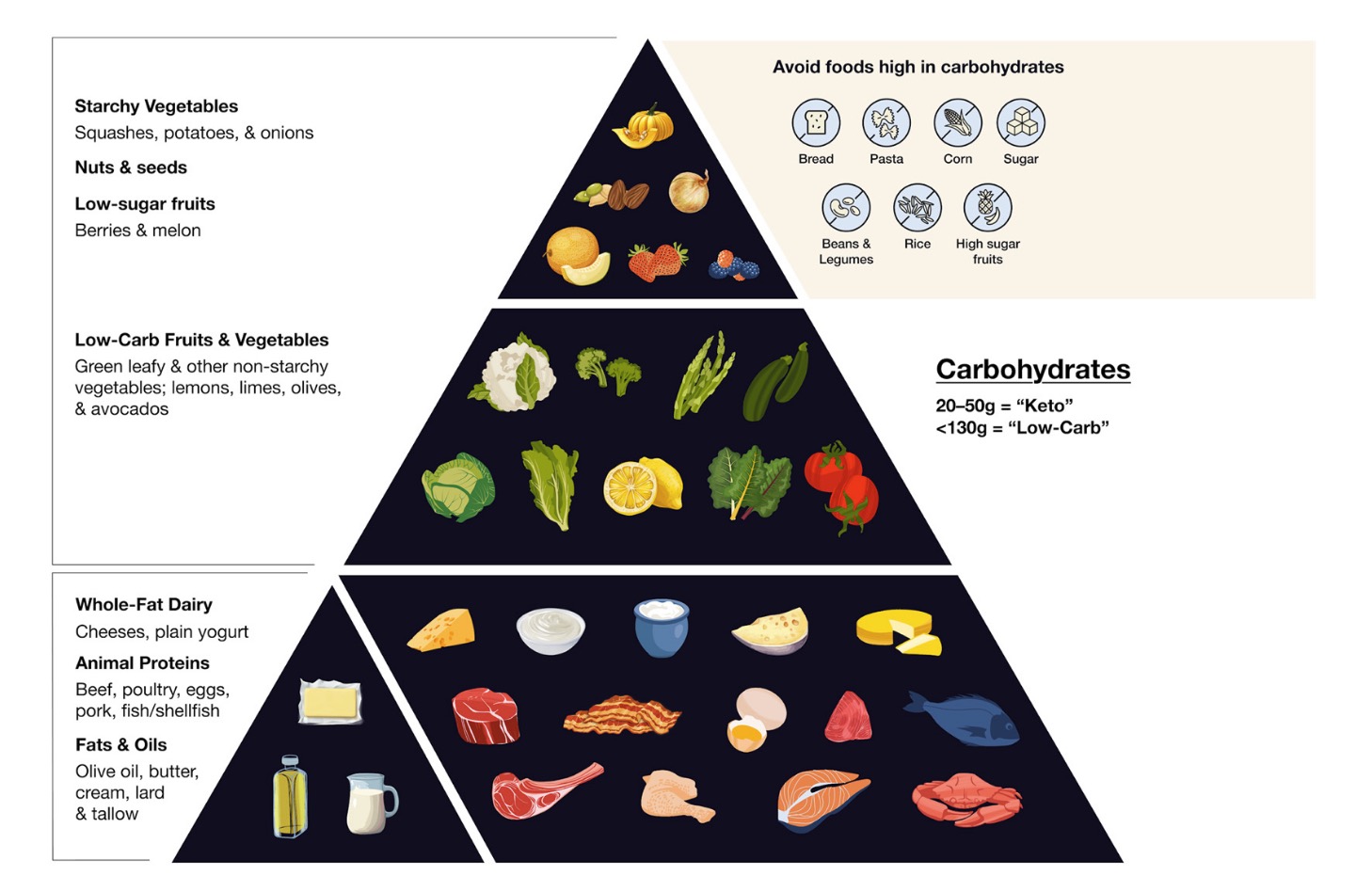
We must first address the distinction between endogenous and exogenous sources of glucose. Clinical trials and epidemiological studies of very low to zero carbohydrate diets support the statement of the US National Academies of Sciences that “the lower limit of dietary carbohydrate compatible with life apparently is zero, provided that adequate amounts of protein and fat are consumed” [8-11]. Even so, despite seemingly safe and increasingly popular, the long-term effects of a truly “zero” carbohydrate diet (without micronutrient supplementation) are difficult to ascertain through controlled experimentation, being only inferred from evolutionary biology, observational studies, and mechanistic data [12-14]. With this caveat, it has now been clearly established in large cohorts of patients, both adult and pediatric, that the oral intake of carbohydrates can be chronically very low (< 5-10% of total daily energy), as long as essential micronutrients are obtained from the underlying food selection and/or supplementation [15-18].
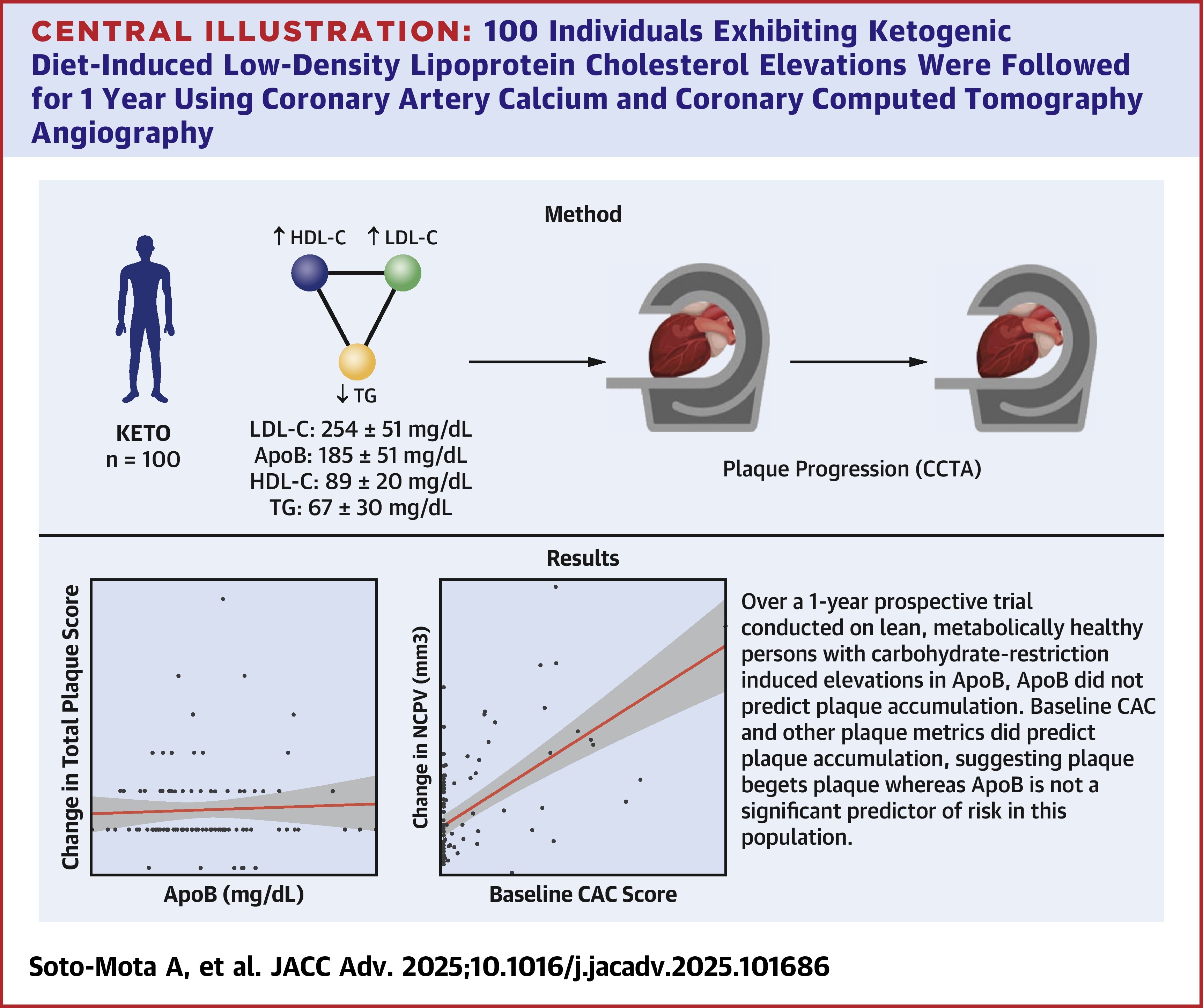
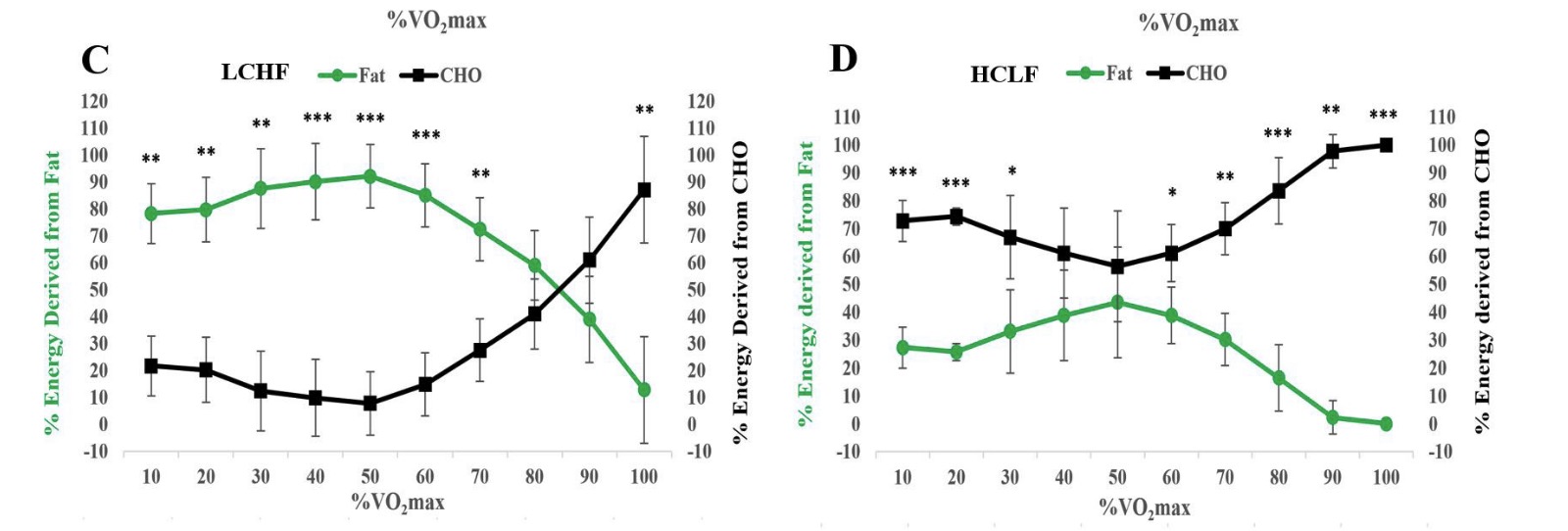
During fasting or in the absence of dietary carbohydrates, a steady-state euglycemia will be maintained in a low but physiological range via hepatic and renal gluconeogenesis from endogenous sources, such as lactate, fatty acids (glycerol), gluconeogenic amino acids and odd chain fatty acids [19-21]. From an evolutionary perspective, a minimal threshold of gluconeogenesis was preserved even after indefinite periods of fasting, questioning whether glucose itself is essential [22, 23]. It was not until the seminal work of Cahill et al. corroborating the remarkable metabolic flexibility of human physiology that the absolute requirements of glucose under compensatory ketosis could be quantified [24]. Drenick et al. demonstrated that, after a 2-month fast in obese subjects, insulin stimulation failed to precipitate hypoglycemic reactions with plasma glucose as low as 9 mg/dl (0.5 mM) [25]. During prolonged fasting, blood glucose levels below 30 mg/dL (1.70 mM) have been sustained continuously for several months without adverse effects [22, 23]. It is apparent that glucose requirements can be significantly displaced by fat-derived fuels, assuming a gradual period of ketogenic adaptation proportional to the degree of glucose depletion [26, 27]. Most human tissues require at least 1 to 4 weeks of strict KD adherence for the effective upregulation of ketone body metabolism, a process that can be accelerated through water-only fasting [28-30]. Without ketogenic adaptation, glucose is indeed the “primary metabolic fuel”, as evidenced by hypoglycemic reactions after accidental secretagogue or insulin overdose in diabetic patients following carbohydrate-rich diets, even under conditions of diabetic ketoacidosis [31-33].
Many clinicians fear ketosis due to confusion with diabetic ketoacidosis, defined by the triad of excessive ketogenesis, metabolic acidosis and concomitant hyperglycemia [34]. A low level of ketones (e.g., < 0.5 mM) prior to initiating carbohydrate restriction indicates that the individual is likely not deficient in insulin and therefore not at risk for ketoacidosis [35]. Clinicians may wish to monitor serum bicarbonate during the early stages of ketogenic adaptation. Ketoacidosis does not occur unless ketones coexist with hyperglycemia and decreasing bicarbonate levels, indicating insulin insufficiency (not to be confused with insulin suppression via carbohydrate restriction, which in turn increases insulin sensitivity, as indicated by lower insulin requirements for euglycemia) [36].
In the context of KMT, evolutionary competition for the limited nutrient supply between the tumor and normal tissues may be potentiated [37]. It is important to clarify that the uninterrupted maintenance of very low glucose levels (< 3 mM) is not realistically achievable for most patients following isocaloric KDs and typically requires prolonged fasting or pharmacological interventions. Fortunately, the anti-tumoral benefits of KMT are hypothesized to arise from pleiotropic regulation of energy sensing and growth signaling pathways (PI3K, AKT, AMPK/mTOR, PGC-1α), inflammation, angiogenesis, and autophagy, not solely as the result of reduced glucose availability with compensatory ketosis, which simply serves as a surrogate marker for successful clinical implementation [38-43].
Ok, this isn't a whole paper by itself, its an appendix of Clinical research framework proposal for ketogenic metabolic therapy in glioblastoma But its so well written, it deserves to be highlighted.
Full Original Paper here: https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-024-03775-4#Sec31 - Supplementary Material 1 - Appendix 1 - Warning - It's a docx document.
references 1-43
- Nakrani MN, Wineland RH, Anjum F: Physiology, Glucose Metabolism. StatPearls 2022.
- Mathew P, Thoppil D: Hypoglycemia. In: StatPearls [Internet]. edn.: StatPearls Publishing; 2022.
- Ritter S: Monitoring and maintenance of brain glucose supply: importance of hindbrain catecholamine neurons in this multifaceted task. Appetite Food Intake 2017:177-204.
- Mergenthaler P, Lindauer U, Dienel GA, Meisel A: Sugar for the brain: the role of glucose in physiological and pathological brain function. Trends Neurosci 2013, 36(10):587-597.
- Luz MR, de Oliveira GA, de Sousa CR, Da Poian AT: Glucose as the sole metabolic fuel: The possible influence of formal teaching on the establishment of a misconception about energy‐yielding metabolism among students from Rio de Janeiro, Brazil. Biochemistry molecular biology education 2008, 36(6):407-416.
- Ghosh A, Cheung YY, Mansfield BC, Chou JY: Brain contains a functional glucose-6-phosphatase complex capable of endogenous glucose production. J Biol Chem 2005, 280(12):11114-11119.
- Brosnan JT: Comments on metabolic needs for glucose and the role of gluconeogenesis. Eur J Clin Nutr 1999, 53 Suppl 1(1):S107-111.
- Lupton JR, Brooks J, Butte N, Caballero B, Flatt J, Fried S: Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. National Academy Press: Washington, DC, USA 2002, 5:589-768.
- Landry MJ, Crimarco A, Gardner CD: Benefits of Low Carbohydrate Diets: a Settled Question or Still Controversial? Curr Obes Rep 2021, 10(3):409-422.
- Goldenberg JZ, Day A, Brinkworth GD, Sato J, Yamada S, Jonsson T, Beardsley J, Johnson JA, Thabane L, Johnston BC: Efficacy and safety of low and very low carbohydrate diets for type 2 diabetes remission: systematic review and meta-analysis of published and unpublished randomized trial data. BMJ 2021, 372:m4743.
- Lennerz BS, Mey JT, Henn OH, Ludwig DS: Behavioral Characteristics and Self-Reported Health Status among 2029 Adults Consuming a "Carnivore Diet". Curr Dev Nutr 2021, 5(12):nzab133.
- Ben-Dor M, Sirtoli R, Barkai R: The evolution of the human trophic level during the Pleistocene. American journal of physical anthropology 2021, 175 Suppl 72:27-56.
- O’Hearn A: Can a carnivore diet provide all essential nutrients? Current Opinion in Endocrinology, Diabetes Obesity 2020, 27(5):312-316.
- Klement RJ: Was there a need for high carbohydrate content in Neanderthal diets? American Journal of Biological Anthropology 2022, 179(4):668-677.
- Westman EC: Is dietary carbohydrate essential for human nutrition? Am J Clin Nutr 2002, 75(5):951-953.
- O’Hearn A, Westman EC, Yancy WS, Wellington N: Nutritional aspects. In: Ketogenic. edn. Edited by Noakes TD, Murphy T, Wellington N, Kajee H, Rice SM: Academic Press; 2023: 71-104.
- Martin-McGill KJ, Bresnahan R, Levy RG, Cooper PN: Ketogenic diets for drug-resistant epilepsy. Cochrane Database Syst Rev 2020, 6(6):CD001903.
- Hagstrom H, Hagfors LN, Tellstrom A, Hedelin R, Lindmark K: Low carbohydrate high fat-diet in real life assessed by diet history interviews. Nutr J 2023, 22(1):14.
- Chourpiliadis C, Mohiuddin SS: Biochemistry, gluconeogenesis. In: StatPearls [Internet]. edn.: StatPearls Publishing; 2021.
- Taherizadeh M, Khoshnia M, Shams S, Hesari Z, Joshaghani H: Clinical Significance of Plasma Levels of Gluconeogenic Amino Acids in Esophageal Cancer Patients. Asian Pac J Cancer Prev 2020, 21(8):2463-2468.
- Rothman DL, Magnusson I, Katz LD, Shulman RG, Shulman GI: Quantitation of hepatic glycogenolysis and gluconeogenesis in fasting humans with 13C NMR. Science 1991, 254(5031):573-576.
- Stewart WK, Fleming LW: Features of a successful therapeutic fast of 382 days' duration. Postgraduate medical journal 1973, 49(569):203-209.
- Thomson TJ, Runcie J, Miller V: Treatment of obesity by total fasting for up to 249 days. Lancet 1966, 2(7471):992-996.
- Cahill GF, Jr.: Fuel metabolism in starvation. Annual review of nutrition 2006, 26:1-22.
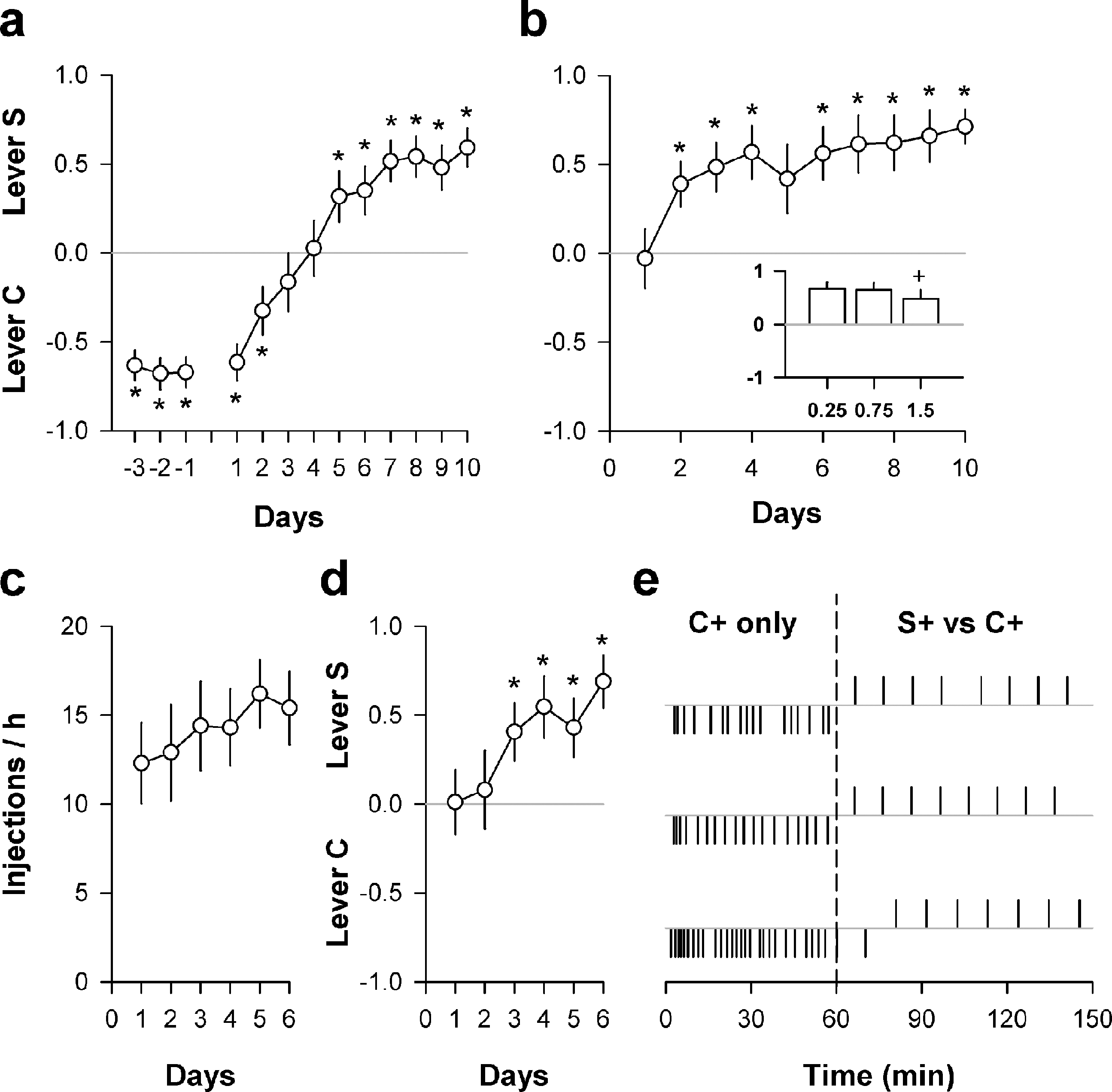
- Drenick EJ, Alvarez LC, Tamasi GC, Brickman ASJTJoci: Resistance to symptomatic insulin reactions after fasting. 1972, 51(10):2757-2762.
- Longo R, Peri C, Cricri D, Coppi L, Caruso D, Mitro N, De Fabiani E, Crestani M: Ketogenic Diet: A New Light Shining on Old but Gold Biochemistry. Nutrients 2019, 11(10):2497.
- Zhang Y, Kuang Y, Xu K, Harris D, Lee Z, LaManna J, Puchowicz MA: Ketosis proportionately spares glucose utilization in brain. J Cereb Blood Flow Metab 2013, 33(8):1307-1311.
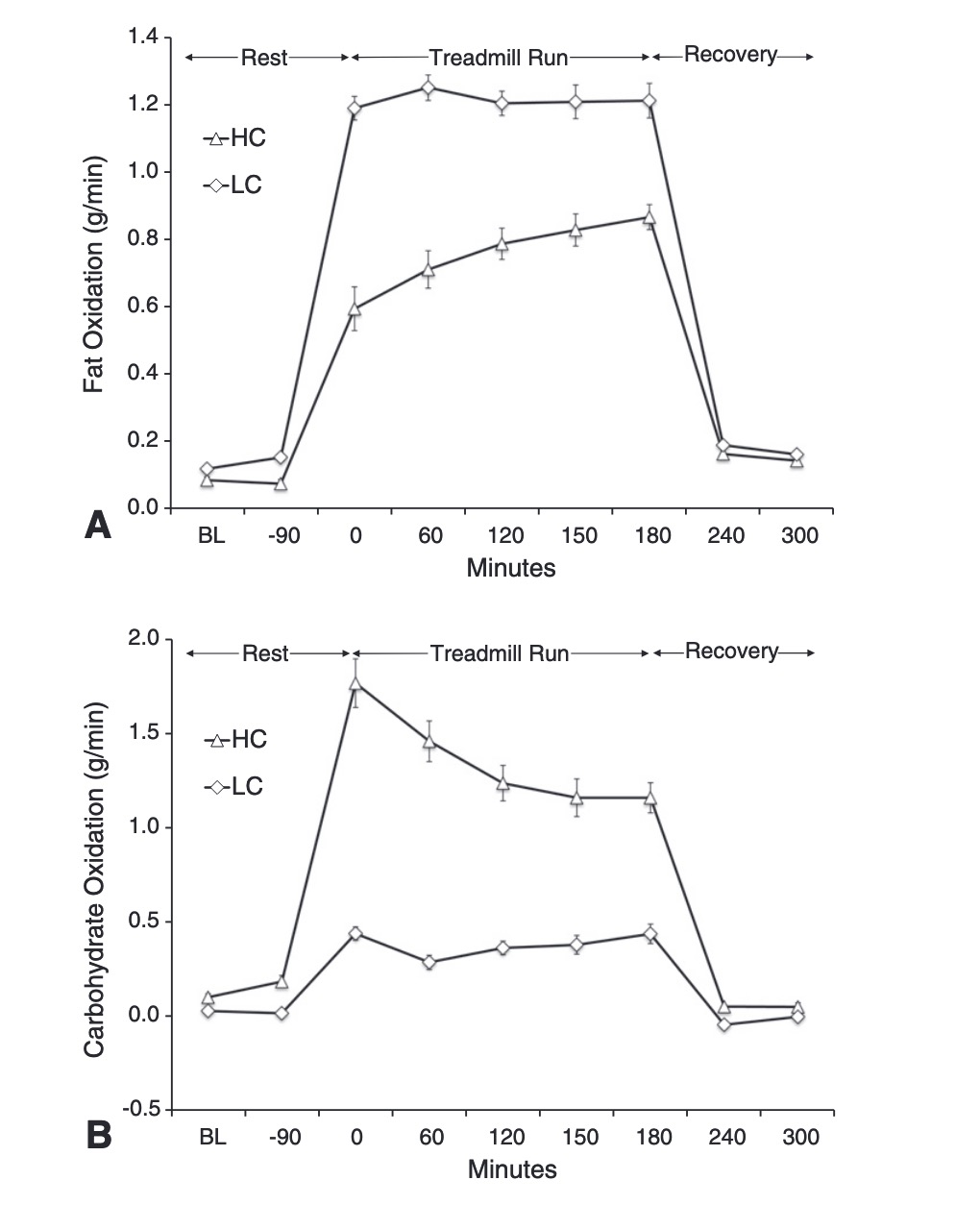
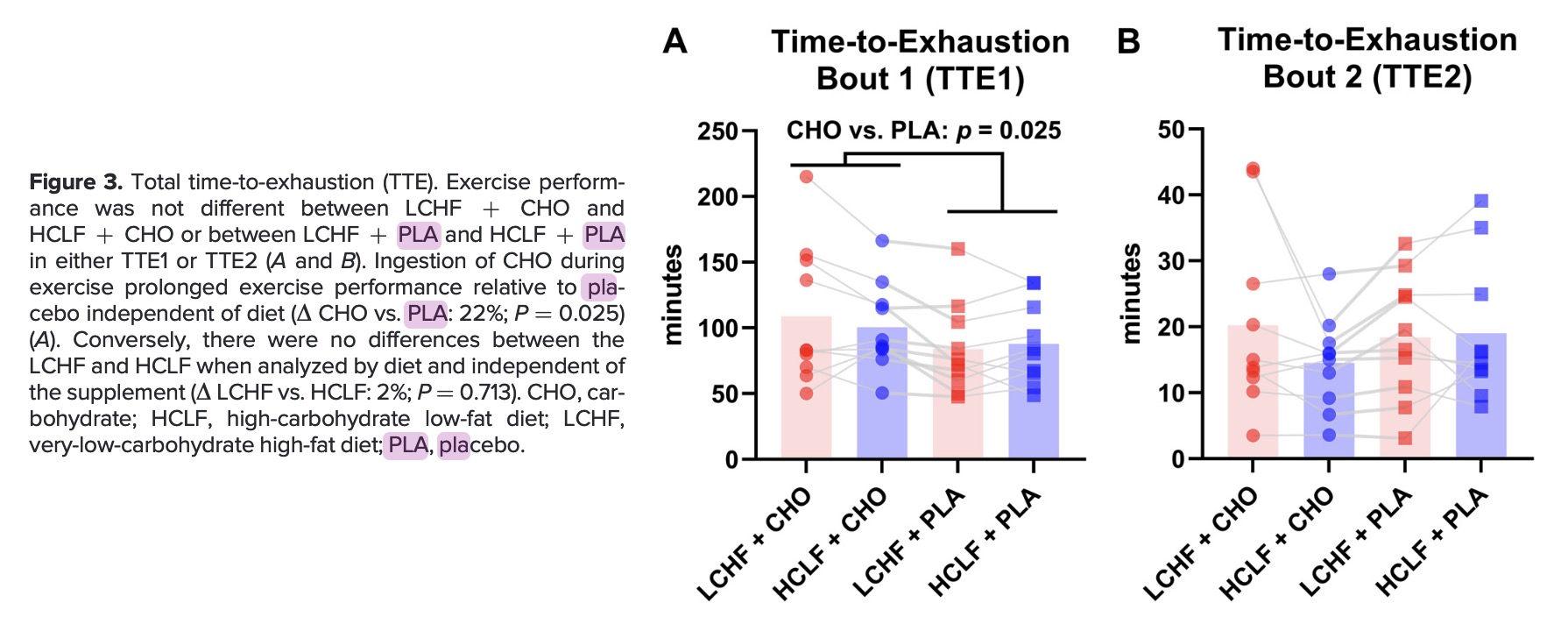
- Burke LM, Whitfield J, Heikura IA, Ross ML, Tee N, Forbes SF, Hall R, McKay AK, Wallett AM, Sharma AP: Adaptation to a low carbohydrate high fat diet is rapid but impairs endurance exercise metabolism and performance despite enhanced glycogen availability. The Journal of Physiology 2021, 599(3):771-790.
- Phinney SD, Bistrian BR, Wolfe RR, Blackburn GL: The human metabolic response to chronic ketosis without caloric restriction: physical and biochemical adaptation. Metabolism 1983, 32(8):757-768.
- Kackley ML, Brownlow ML, Buga A, Crabtree CD, Sapper TN, O'Connor A, Volek JS: The effects of a 6-week controlled, hypocaloric ketogenic diet, with and without exogenous ketone salts, on cognitive performance and mood states in overweight and obese adults. Front Neurosci 2022, 16:971144.
- Pathak RD, Schroeder EB, Seaquist ER, Zeng C, Lafata JE, Thomas A, Desai J, Waitzfelder B, Nichols GA, Lawrence JM et al: Severe Hypoglycemia Requiring Medical Intervention in a Large Cohort of Adults With Diabetes Receiving Care in U.S. Integrated Health Care Delivery Systems: 2005-2011. Diabetes Care 2016, 39(3):363-370.
- Chantzaras A, Yfantopoulos J: Evaluating the Incidence and Risk Factors Associated With Mild and Severe Hypoglycemia in Insulin-Treated Type 2 Diabetes. Value Health Reg Issues 2022, 30:9-17.
- Ben-Ami H, Nagachandran P, Mendelson A, Edoute Y: Drug-induced hypoglycemic coma in 102 diabetic patients. Archives of internal medicine 1999, 159(3):281-284.
- Dhatariya KK, Glaser NS, Codner E, Umpierrez GE: Diabetic ketoacidosis. Nat Rev Dis Primers 2020, 6(1):40.
- Cooper ID, Brookler KH, Kyriakidou Y, Elliott BT, Crofts CAJB: Metabolic phenotypes and step by step evolution of type 2 diabetes: A New paradigm. 2021, 9(7):800.
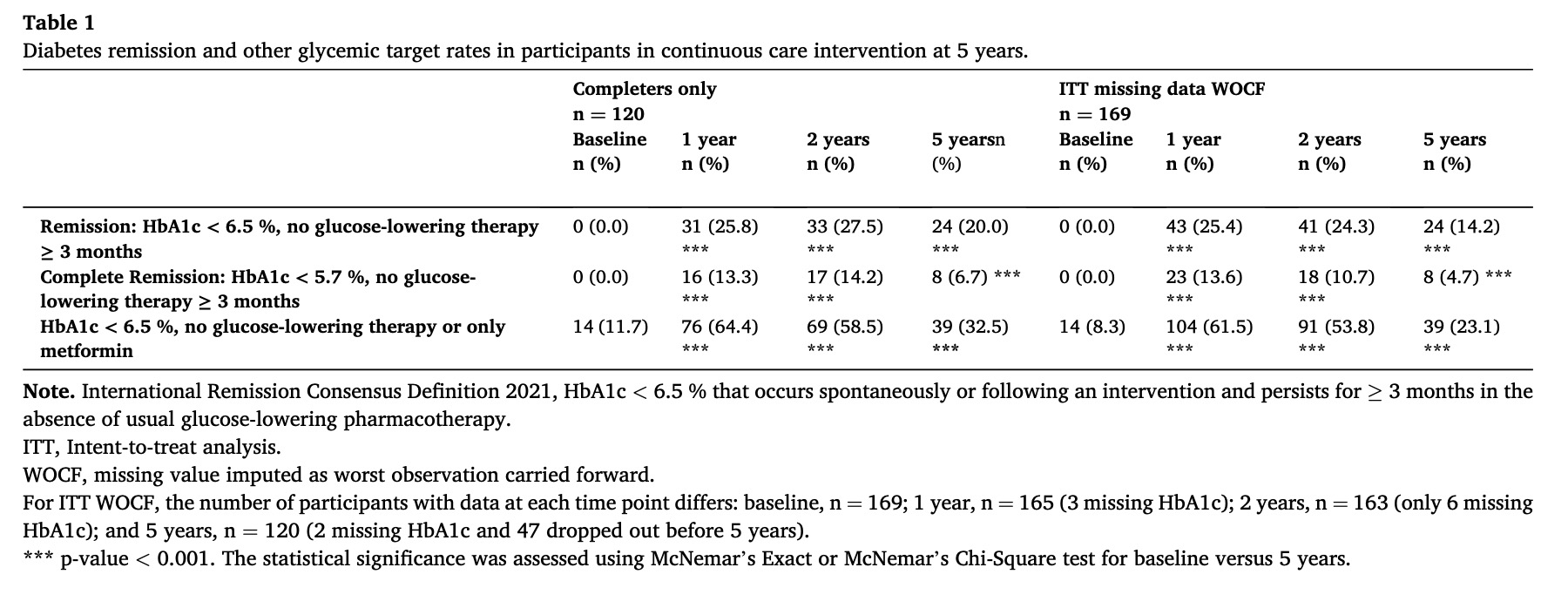
- Yuan X, Wang J, Yang S, Gao M, Cao L, Li X, Hong D, Tian S, Sun C: Effect of the ketogenic diet on glycemic control, insulin resistance, and lipid metabolism in patients with T2DM: a systematic review and meta-analysis. Nutr Diabetes 2020, 10(1):38.
- McCall AL, Fixman LB, Fleming N, Tornheim K, Chick W, Ruderman NB: Chronic hypoglycemia increases brain glucose transport. Am J Physiol 1986, 251(4 Pt 1):E442-447.
- Mukherjee P, El-Abbadi MM, Kasperzyk JL, Ranes MK, Seyfried TN: Dietary restriction reduces angiogenesis and growth in an orthotopic mouse brain tumour model. Br J Cancer 2002, 86(10):1615-1621.
- Mukherjee P, Mulrooney TJ, Marsh J, Blair D, Chiles TC, Seyfried TN: Differential effects of energy stress on AMPK phosphorylation and apoptosis in experimental brain tumor and normal brain. Mol Cancer 2008, 7:37.
- Mulrooney TJ, Marsh J, Urits I, Seyfried TN, Mukherjee P: Influence of caloric restriction on constitutive expression of NF-kappaB in an experimental mouse astrocytoma. PLoS ONE 2011, 6(3):e18085.
- Shelton LM, Huysentruyt LC, Mukherjee P, Seyfried TN: Calorie restriction as an anti-invasive therapy for malignant brain cancer in the VM mouse. ASN Neuro 2010, 2(3):e00038.
- Zhou W, Mukherjee P, Kiebish MA, Markis WT, Mantis JG, Seyfried TN: The calorically restricted ketogenic diet, an effective alternative therapy for malignant brain cancer. Nutr Metab (Lond) 2007, 4:5.
- Wong W: Mitochondrial fission fueled by fasting. Sci Signal 2023, 16(797):eadk1008.
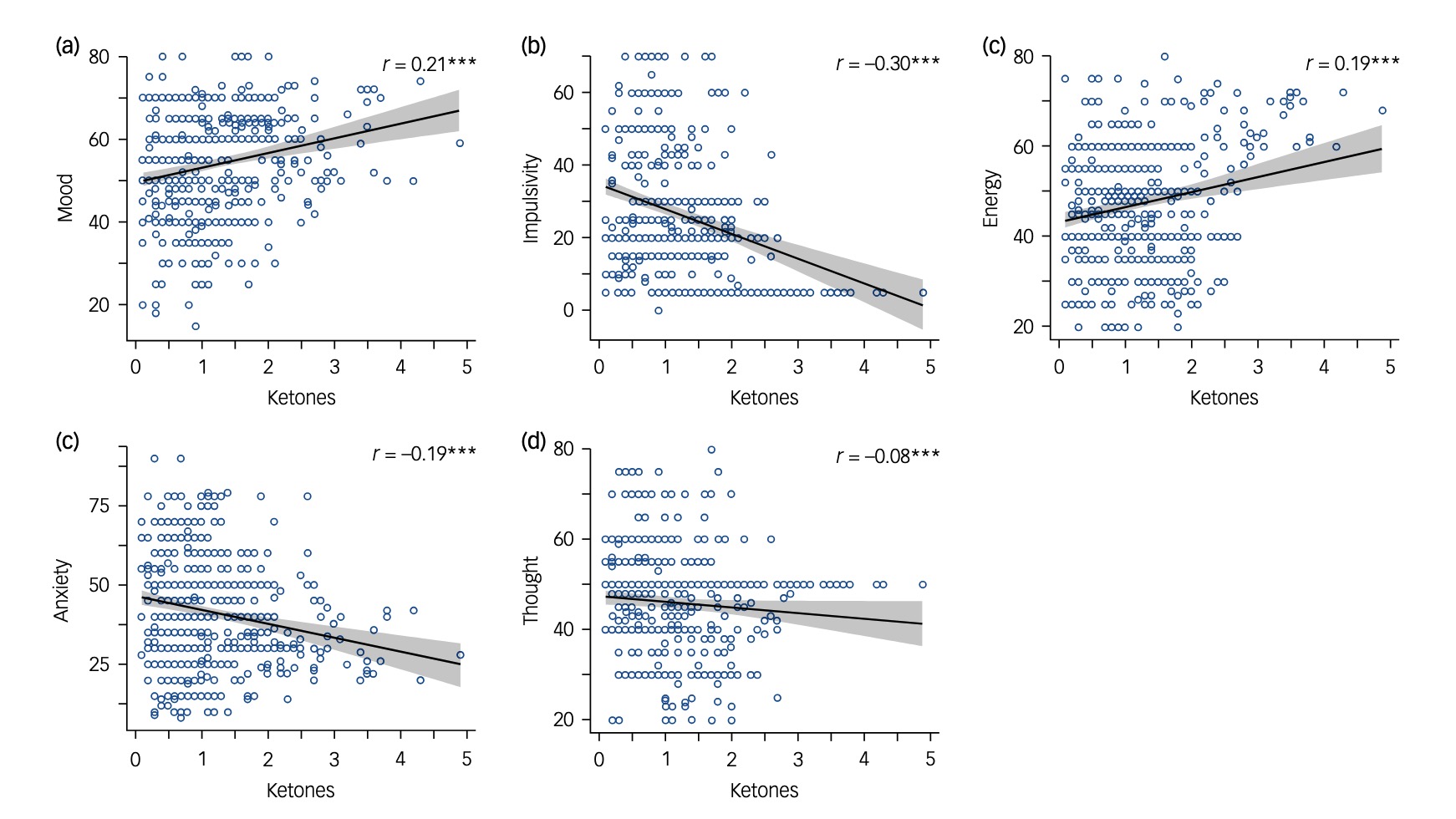
The image in the post is from Resistance to Symptomatic Insulin Reactions after Fasting which is reference 35.